This project was carried out with the invaluable collaboration of
 and
and 
please see a full listing of all contributors at the bottom of this post
Project Outline
With the CoVid19 pandemic hitting South Africa hard and starting to take root in the Eastern Cape, our medical staff at the local Livingstone Hospital are under enormous strain and this project was aimed towards helping to protect healthcare workers at the frontline who rely heavily on PPE. As such, we received an urgent appeal from Anaesthetist Dr Lorenzo Boretti through Orthopaedic Surgeon Dr Bryan Theunissen regarding challenges faced by the in-theatre Anaesthesia teams in their CoVid theatre.
The challenge is to contain aerosolized droplets from patients with possible CoVid19 virus infection during procedures to ensure that the theatre staff assisting in the operation are minimally exposed to these droplets.
Design & Manufacture Timeline
Thursday 2nd April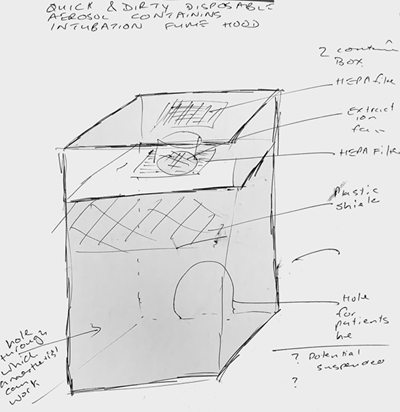
The call came through on Thursday morning 2nd April, and the AEDG Team as well as multiple contributors from our network of both academic and private sector experts immediately started an online process of working on a possible solution to the challenge. Huge thanks must go to all contributing individuals who will be listed at the end.
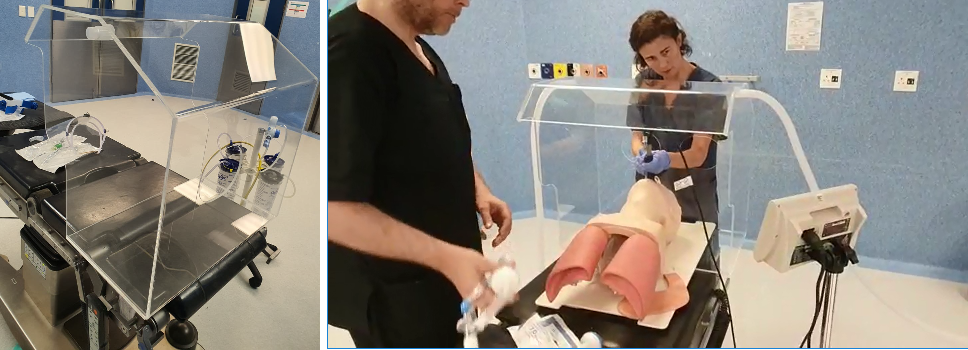
Initial information was difficult to come by as the medical staff at Livingstone are constantly on call dealing with the crisis, so a basic set-up was ultimately agreed upon as a starting point which could be updated as more information came to hand. An initial conceptual idea was sent through by Dr Theunissen as shown...
Challenges #1
-
Due to complete lack of available funding, the team had to fashion a solution from readily available material - we had wood (not an option), perspex (not ideal but would work for an initial prototype) and a 3D FDM printer with PLA filament (again not ideal but would suffice)
-
The resultant Intubation Structure would be needed ASAP as the team were undergoing anything up to 10x procedures per day on a consistent basis
-
Availability of the correct filters was non-existent & the theatre extraction units were already tied up according to initial info
Strategies #1
-
We sourced (and were sent) as much information about existing similar structures on the internet - there are many, including some open-source designs from both high-brow academic institutions as well as individuals...this gave us a starting point
-
We used the measurements of the head of a large academic (no names mentioned!) as a base model for bounding dimensions as a worst-case scenario
-
Much discussion went on through the online group iro sterilization options and filter options in the structure - these were a serious and very expensive option so appeared at this stage to be a serious stumbling block unless alternative options could be found
-
An early assumption was that the structure would have to be disassembled after each procedure for sterilization processes, so the design would have to be completely collapsible.
Design Process #1
-
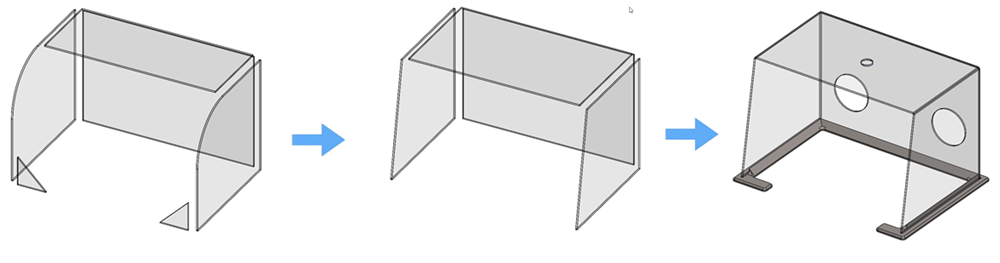
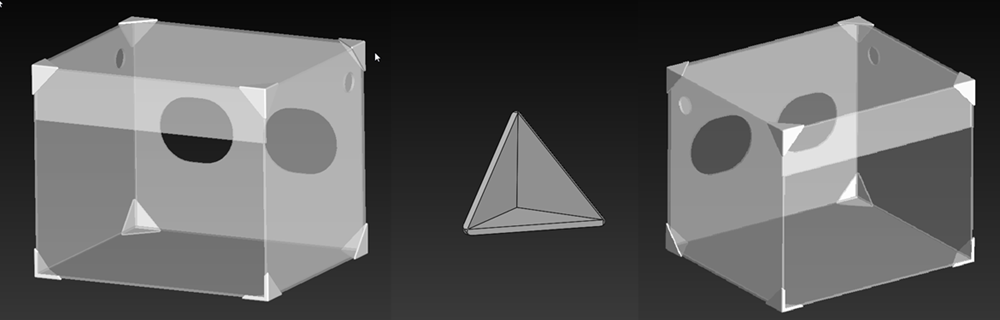
A basic box structure consisting of collapsible perpex panels and a 3D printed frame was initially designed pending further feedback
-
Initial considerations were made for a modularized concept whereby the filtering module would be an entirely separate but modular connection to the main Intubation Box structure which would fit over the patient's head.
-
Cecil Frost from Shibah Engineering (and an NMU Mech Eng alumni) would visit the Theatre on Friday morning and would be able to give more detailed feedback, after which the initial design could then be updated to those specifications.
-
In the meantime, options for the material available were sought and by early afternoon, a basic mock-up had been created and developed utilizing simple panels and a 3D printed base for stability...
-
Circular holes were provided at the back of the structure to provide access from the Anaesthetic staff members
-
A small circular hole was provided on the top plate of the structure to provide evacuation to either a filter module or to a vacuum extraction unit
-
as the day wore on into the early hours of the next morning, and after several online meetings, further 3D printed cage elements were developed and included into the assembly structure
-
two holes were created at the top back of the side sections to integrate possible vacuum evacuation flow through the structure pending feedback the next day
-
a frontal flat 'goalpost' section was included to provide a base for 'tacky tape' inclusion of a frontal plastic curtain in the event it may be needed
-
for the moment, the sterilization and evacuation module was put on hold until we had more detailed info from the theatre
-
a tired team closed up shop at around 03:30 on Friday morning
Friday 3rd April
Early on Friday morning, Cecil met with Dr Boretti and visited the Theatre to observe training on theatre set-up - immediately, some challenges came to hand that we were completely unaware of including some positive aspects which ease the design process as well; the design would nevertheless have to be changed quite significantly...
Also, adding to the mix were some additional concepts that had arisen overnight as people applied their minds to the challenge. However, it was decided to put these on the backburner until later down the line as they would need quite specific material and extrusions that were simply not available immediately and would have to be purchased, prolonging the period until an actual prototype could be produced.
Challenges #2
-
Firstly, the width of the operating bed was considerably smaller than we had anticipated intially, which would require a slimming down of the entire structure to avoid it protruding beyond the bedspace and making it unstable
-
Next, the medical staff would need an unobstructed view of the patient's head at all stages of the procedure, so the 3D-printed support cage structure would have to go
-
There was no space for the 3D-printed base, so that would have to go as well...but, as a positive, the structure would not be disassembled after each procedure
-
Evacuation holes would have to be relocated to the top-back sides of the structure to accommodate a plan Cecil had come up with to set up a piping system to integrate with the AC system's exhaust due to non-availability of an additional vacuum extractor - this did away with the evacuation module & the filter challenge on the structure itself, another positive iro simplifying the design
-
The access holes at the back would need a redefined shape to accommodate differing hand sizes and better hand movement around the patient's head
-
To balance the airflow for extraction, a small frontal plate would need to be inserted above the patient's head

Strategies #2
-
The bed size change and the removal of the 3D-printed support was the biggest challenge as this impacted not only on the geometry of the entire structure, but also on its structural stability, as the team had to work with whatever material we could find in our Lab Space.
-
A major boon was the fact that the structure did not have to be disassembled after each use, as that had really complicated things iro the initial concept.
-
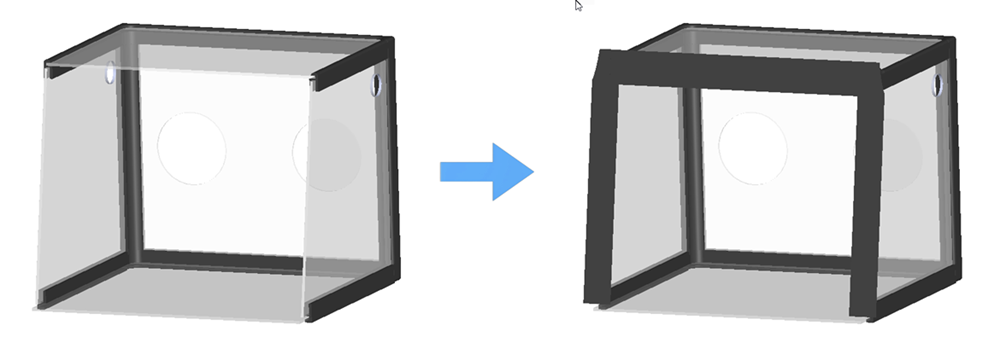
After yet another online meeting between those most closely involved in the project, the design was simplified quite considerably to a very simplified transparent box with 3D-printed corner brackets - the whole structure would be held together by glue and silicone seals
-
The corner brackets now needed some serious consideration as they would have to impart a lot of the structural stability of the entire structure - before this had been taken up by the base and the cage
Design Process #2
-
The initial basic box structure was retained with the easy-to-achieve updates like the repositioning and sizing of the holes achieved first, and then the frontal plate inserted as an additional feature
-
The original more-complex corner brackets were simplified considerably to a minimized suitcase-corner-bracket style component that could be directly bonded onto the outside of the perspex plates imparting additional stiffness to the structure... a far neater, more satisfying result overall.
-
This second iteration was completed well into the early hours of Saturday morning in preparation for manufacture and build on Saturday.
Saturday 4th April
Manufacture Process

This, we anticipated, was going to be the most straightforward task, but it was to prove to be a constant slog against every possible hurdle that could be thrown at the team.
eNtSA very kindly offered to water-jet cut the panels for us using our in-house facilities, and both Riaan Opperman and Riaan Brown (again both NMU alumni) made themselves available to facilitate this.
This is where things started to go a little pear-shaped...
First-off, the material we thought we had to hand in our Labs was considerably less than anticipated; and not only that, it was also considerably thinner than we had expected.
Houston-We-Have-A-Problem 01 - Material Hunt:
Between Zaahid, and the two Riaan's, began a hunt through all the North Campus Labs for suitable transparent panels.
An email and WhatsApp appeal was also circulated to all staff to look for available transparent sheets - and the staff responded magnificently with a variety of comebacks from Industrial Engineering (Dr Anne Lourens) to Mechatronics Engineering (Prof Farouk Smith) to Innoventon (Dr Shawn Gouws), all offering up what they had available. A huge thanks to all...
Fortunately, a sheet was scavenged from scrap within the Water-Jet Cutting Lab, although of a different thickness to our left-over pieces, and the team was able to cut the profiles so that Zaahid could return home to put everything together...big thanks to both Riaan's and eNtSA for their quick assistance on this...
Houston-We-Have-A-Problem 02 - Stubborn Film:
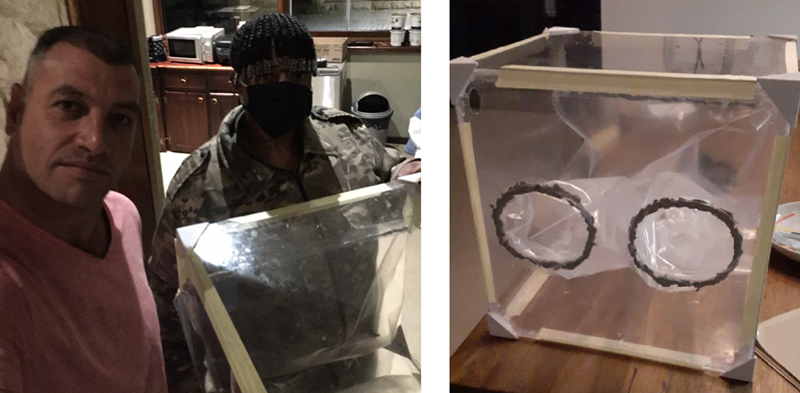
Zaahid began the process of build-up while waiting for the 3D prints of the corner brackets to finish.
Our next major challenge only became evident when Zaahid got home and made himself comfortable for the build. The covering film on the perspex sheets seemed incredibly stubborn to come off.
As we were to find, these panels were very old and the film had become very accustomed and attached to its host.
A whole variety of tricks, Google searches and persuasion didn't help, and poor Zaahid spent well over 5 hours slowly extracting the film bit by bit, losing not only valuable time but several finger nails along the way!

In the meantime, in a parallel operation, Charl was preparing plastic film hand tunnels and a frontal curtain for the box at his house using plastic film that we had scavenged off our supply of carbon rolls, in the event that the theatre staff would need this to help further protect them from potential exposure.
These would be attached to the outside of the box using tacky-tape surrounds and threaded through the hand-holds into the structure. They were made overlong to allow the theatre staff to cut them to their own sizing in the initial testing.
These were ready late Saturday afternoon and dropped off at Zaahid's house so he could add them to the final box when done....

As the night wore on until early hours, 3D printed brackets were printed out and Zaahid started glueing the panels together using the completed brackets.
The process would continue on Sunday morning....
Sunday 5th April
Sunday was to prove to be a long frustrating day of waiting for 3D prints and for glue and silicone to set...again, being limited to what was available and to-hand in the AEDG Lab was severely limiting...
Slowly the structure took shape and was taped into position while the rest of us waited and waited...

Not having a reasonable superglue to hand, meant that the curing of the available glue was taking forever, but eventually the structure was stable enough for Zaahid to attach the plastic film tunnels & fonrtal curtain to the structure & to stick his head into it so we could finally get a realworld gauge of the volume and fitment of the box - it was looking good considering...


The video below shows a 360degree walkaround of the completed box prior to delivery:
Further clean-up and reinforcement was carried out late in the afternoon as well as further application of silicon seals in preparation for delivery to Dr Boretti.
Houston-We-Have-A-Problem 03 - Shutdown Restrictions:
The next challenge we encountered was that the structure had to be delivered across town with the two points being as far apart as luck would allow! The initial plan of Zaahid running the blockade was initially entertained, but his potential arrest at any of several possible SAPS roadblocks would create a severe obstacle to our plans.
As such, a further call was put out amongst our network, and within 10 minutes, Prof Danie Hattingh had come up with a solution via one of his contacts in the SAPS. Offduty W/O Corne Strydom kindly offered to pickup the structure and deliver it to Dr Boretti's residence that night. By 21:00 it was on its way and in the doctor's hands by 22:00...huge thanks to both Danie and Corne for their assistance in this regard.
Monday 6th April
Early Monday morning, the version 2.0 box was put through its paces in a training process in-theatre where the entire process of intubation was gone through to assess where problem areas may exist. With Cecil being present throughout, the following issues came to light...
Design Process #3
The issues picked up in the first in-theatre training test were the following:
-
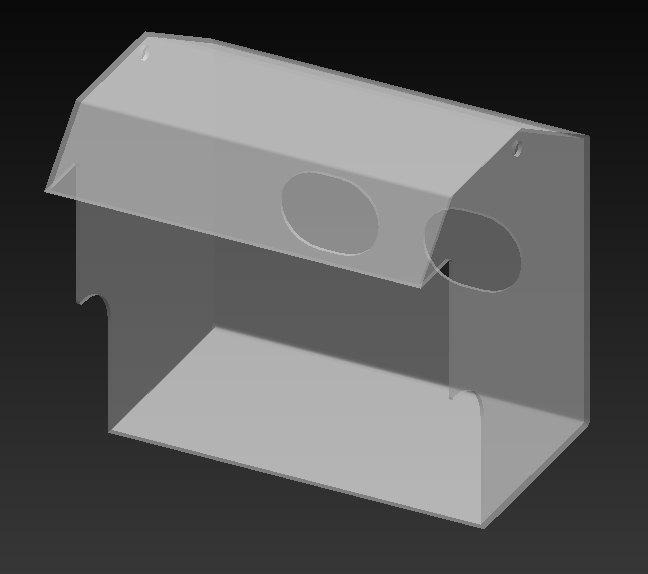
the structure was too low to allow vertical extraction of intubation devices, so that would have to increase
-
the frontal panel needed to be inclined forward to allow suitable access and extraction of intubation devices
-
a rear top viewing panel would need to be included for clear vision of the anaesthesia staff to the patient's head
-
the evacuation holes would have to be changed to integrate with the vacuum extraction unit
-
cut-outs would be needed to allow the patentient's head to be positioned deeper into the box
-
the plastic film tunnels and curtain would not be needed
-
the next device would need to be manufactured from material that was medically compliant
-
the structure needed better stability, which would be achieved with thicker material & a better manufacturing procedure
Despite the fairly significant list, these updates were quickly achieved and were available within the hour iro the geometry changes and a Version 3.0 prototype was drawn up.
Houston-We-Have-A-Problem 04 - An Empty Stockpile!:
The next challenge we faced was the fact that:
-
we were completely out of available material from our Labs
-
the material required for the structure had to be quite specific iro the environment it would be working in
-
it would be costly!
Fortunately, Cecil had contacts through his company Shibah Engineering and was able to arrange the manufacture at a local company whereby they would able to source the correct material, cut it according to specification, bend it and glue it and hopefully it would be ready by late the next day.
Tuesday 7th April
We all waited in some nervous anticipation the whole day for news on the outcome - delays in sourcing and manufacture would see the structure only available early the next day; there was nothing to do but wait...
Word did come through though that the Intubation structure had attracted attention from hospitals in East London as well as in Kwa-Zulu-Natal too, so there seemed to be some legs in it if it met with approval from the theatre staff iro its functionality...
Wednesday 8th April
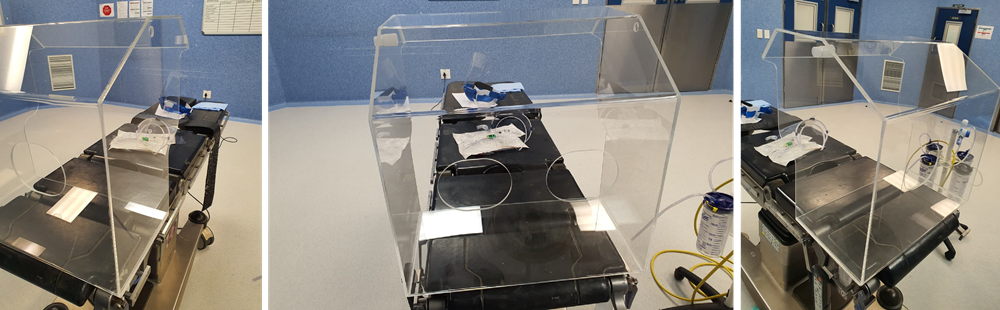
The completed structure was picked up early in the morning and taken back to the hospital for further testing during in-theatre training.
The video from the training is shown below - the changes seemed to have worked to the satisfaction of the theatre staff, which was a huge relief!
Our job at this point seems to be done, pending any further feedback - we can only hope that this in some way aids towards the protection of our brave medical staff.
Well done to all involved!
Thursday 9th April
EP Herald article - click the link on the left to read more about the NMU initiatives iro the CoVid19 response
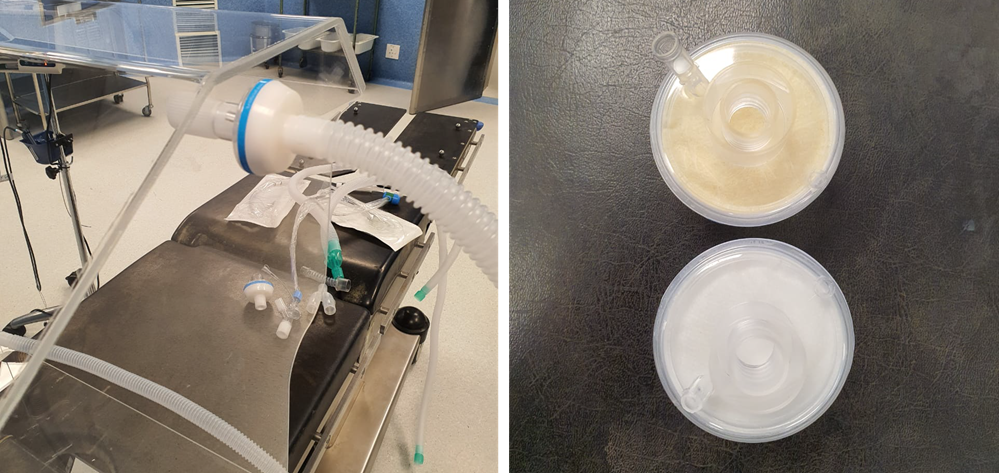
The adaptors for the attachment of the vacuum evacuation tubes were fitted this morning, and linked up to the vacuum unit together with filters on either side of the structure.
An inpromptu test using a cigarette to generate smoke was carried out to see the flow of the vapour through the structure...photos and video below - further tests to be conducted...an interesting outcome after the use of one cigarette was the state of the filter compared to an unused one. (there are two either side, so this would represent effectively half a cigarette's effects! - enjoy your next drag you pack-a-day fiends!)
Two additional small jobs arose from this morning's test: 3D prints of an adapter for the vacuum extractor and an extraction cover for a surgical saw device for both neuro-surgery and orthopaedic processes.
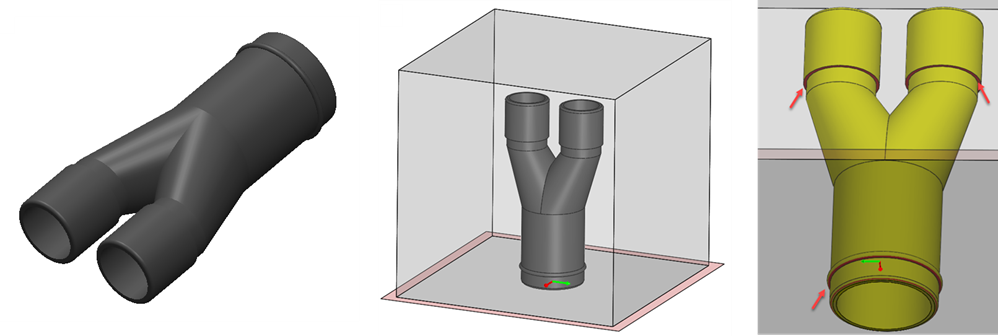
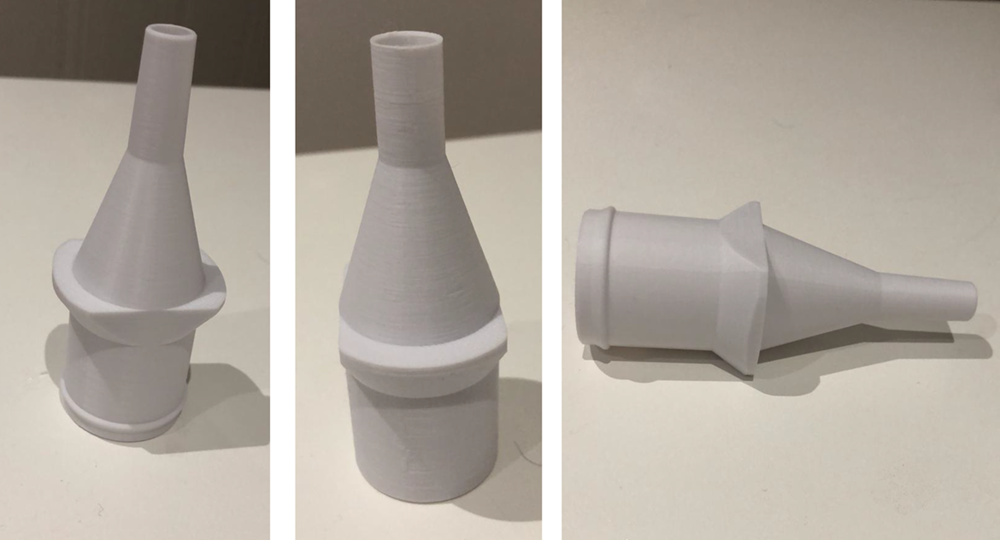
Vacuum Adapter:
This adapter was urgently needed to create an additional vacuum extraction point onto the existing vacuum to connect hosing to the Intubation Unit - it was a fairly simple 2-into-1 structure that connected directly into existing vacuum units as well as evacuation hoses.
The major challenge was to ensure that fitment geometry was not interfered with and that the design was orientated for 3D print to ensure a minimum amount of support material in the print to ensure that post-processing was reduced and the finish was not unnecessarily compromised. We also wanted to ensure no internal support in the vacuum channels.
This required a simple solution of some well-placed chamfers and orientating the structure stading-up & the print was on its way, and woud be ready by late evening...
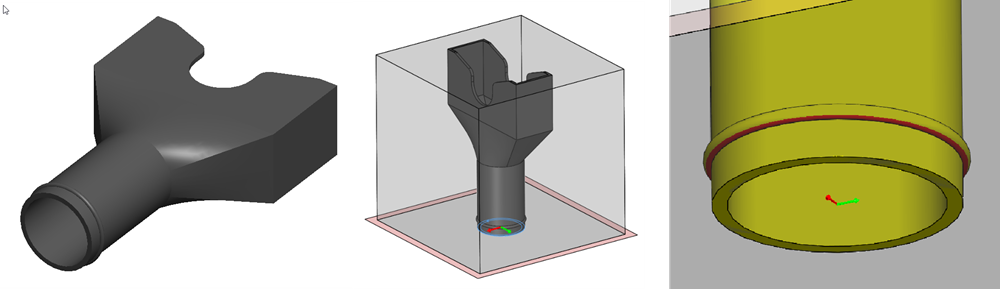
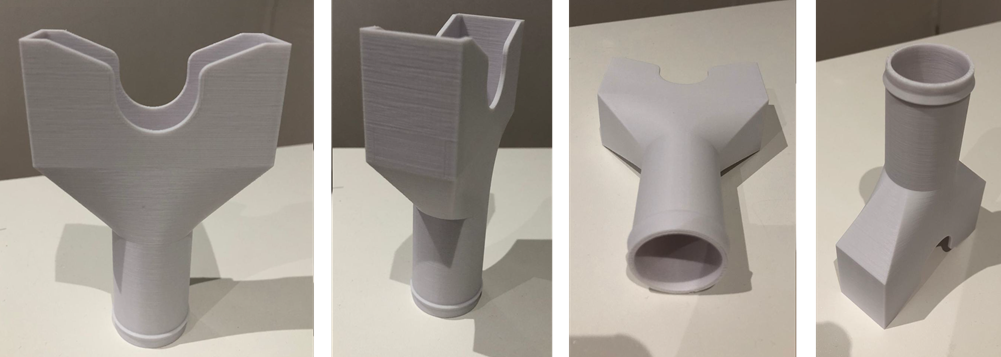
Extraction Cover
This extraction cover was needed for a surgical saw used in both neuro-surgery and orthopaedic processes to extract local debris from the point of incision to the vacuum extraction unit. Again, it was a fairly simple structure and required only consideration iro reducing post-processing issues in the 3D Printing process.
Much like the vacuum adaptor, the only challenges here were orientation and reduction of support material by a few well-placed geometric changes. The print would hopefully be completed overnight and ready for implementation in theatre tomorrow morning.
Friday 10th April (Good Friday)
Happy & safe Easter weekend to all...the vacuum adaptors required for the vacuum extraction unit came out the printer overnight and were delivered early on Good Friday for inclusion into the extraction unit.

The extraction covers are currently printing and should be ready later today...
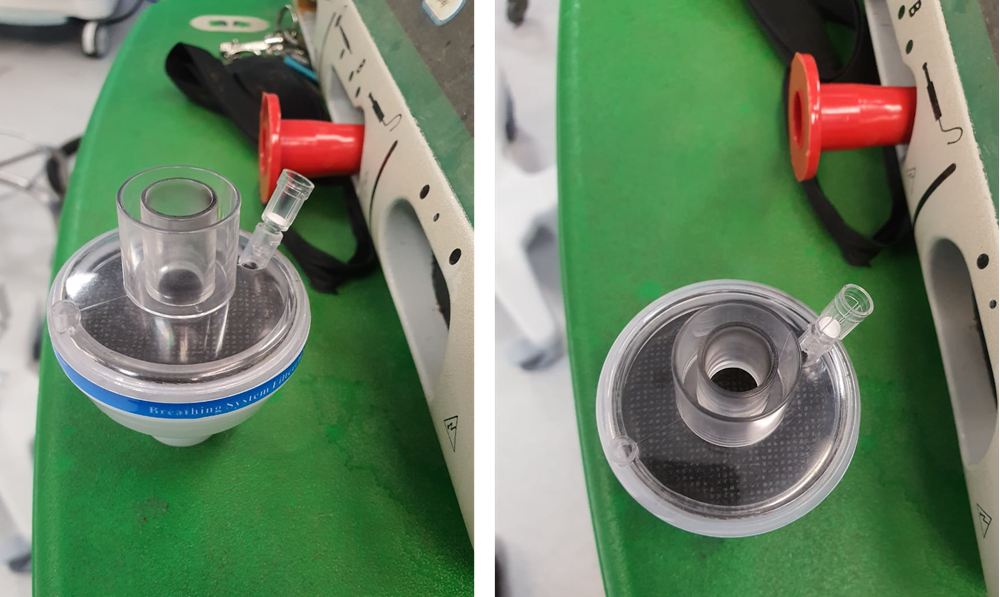
Suction Waste Collector Connectors
In addition to these components, an additional request came through early this morning for two other components - which are connectors for a suction waste collector attached to vacuum extraction units during operation procedures.
Adaptors for both inlet and outlet nozzles are required and were design and adapted for 3D printing outputs - both are very similar with slight geometric differences.
Schematics of one of the designs can be seen below, as well as orientation within the 3D Printer to ensure that there is no support material to complicate post-processing.
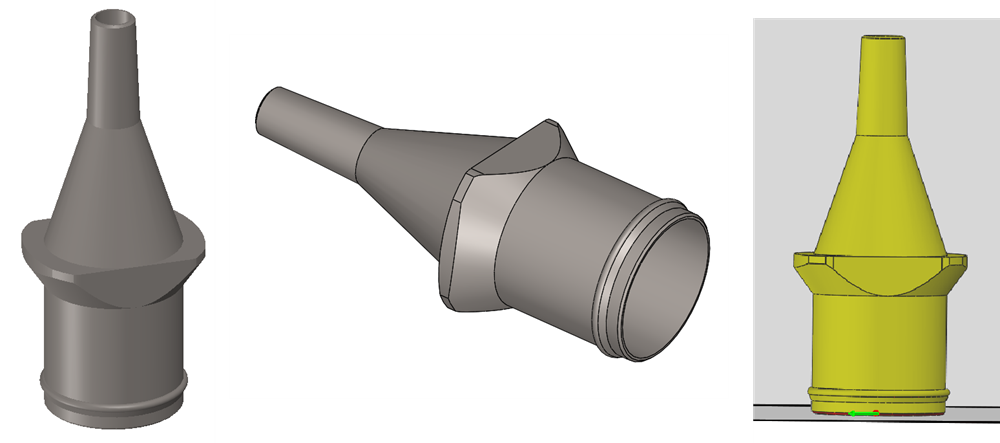
The first of these connectors were ready by mid-afternoon...priority was given to these as they needed to be integrated into the vacuum extraction unit to complete the whole vacuum extraction sub-system.
Saturday 11th April
Suction Waste Collector Connectors
The suction waste collector inlet anbd outlet connectors were both ready for fitment early Saturday morning to the suction waste collector caps, and they all fitted just perfectly which was a huge relief. See the photos below of the units fitted into the collector cap...

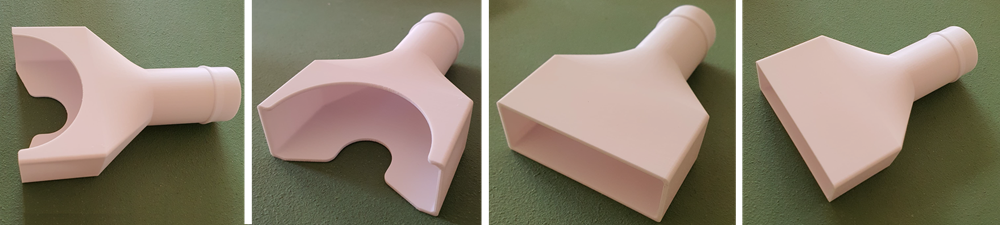
Extraction Covers
This extraction cover prints were also completed late on Saturday after the more urgent comnponents were done. After a somewhat troublesome print, we managed to get them done, and ready for further testing on Monday at the hospital.
The plan going forward was as follows:
-
The units would be taken to Livingstone Hospital early Monday morning where the Intubation Box together with the entire assembled vacumm extractor set-up would be tested in theatre in a mock operation
-
Later in the week, this would then be tested in the non-Covid theatre in an actual procedure to test its viability and functionability, and then further decisions taken from point on
-
The extraction cover for the surgical saw would als be tested in-situ later in the week, and then further decisions also taken in that regard.
Sunday was going to be a day of rest...
Monday 13th April
The various in-line connectors in the vacuum extraction system were all installed and connected through to the Intubation Unit for testing once more in-theatre, and everything seemed to work to perfection.
Using some simple smoke emitting options, replication of a patient's exhalation was simulated relative to the position of the head within the unit, and the extraction worked well - there appeared to be no escape of smoke from the front of the unit, nor through the hand-holes at the rear, so so-far-so-good...
The test is shown in the video below...and below that the state of the filters post-test.
Thurs-Friday 16-17th April
Extraction Cover updates
Some small updates were needed on the Extraction Covers, and these were readied for print late on Thursday afternoon for overnight run. An additional item, a slightly different version of the Extraction Cover for Extubation purposes, was also quickly created and also run in the same print.
These were completed Friday afternoon for pick-up and are shown below - these will be further tested in in-theatre tests early next week.
Sat-Monday 18-20th April
Really great news from the weekend was that the project had secured funding to provide for multiple units for the PE Hospital Complex; this funding would become available soon and the whole process of manufacturing the Intubation Units needed would begin soonest via a local PE company.
Tuesday 21st April
Further testing of the Intubation Unit was carried out in-theatre at Livingstone Hospital by SafeTech using a particle counter provided by Aspen Pharmaceuticals. This test proved successful in reducing aerosolized contamination significantly, with the flow characteristics due to extraction following expectations.
Next would be a basic CFD analysis over the next few days to verify the flow trajectories...
Wed-Monday 22nd April-1st May
An initial baseline CFD was carried out with satisfying results iro the flow trajectories showing no escape of air through the front of the unit nor through the rear hand holes and the extraction holes serving their purpose; much further work has still to be done in this respect, but the initial results were promising and confirmed those tests carried out in-theatre iro the flow through the unit.
8th July brings a Step Forward...
After over two incredibly frustrating months of dragging & kicking heels while dealing with various SAHPRA red-tape issues iro registering medical products before they can be installed in hospitals and used by medical staff, all the while knowing that local theatre staff are being continually exposed to imminent danger on a daily basis by a spiking pandemic, things moved forward as Shibah were able to bring Norpharm on board. This enabled manufacture and distribution under their licence and manufacture began by Shibah Engineering on multiple units to be installed in the local hospitals.
Further developments are also in play iro getting the device & system more widely utilized...updates on this a little later...
Monday 13th July - First Units Delivered
Finally, success after a frustrating delay, as the first 4x units plus all their accessories were delived by Cecil to Livingstone Hospital and immediately taken through to the theatres for testing. Manufacture of the remaining units will continue, and testing in-theatre will take place over the next few days.

(l-r) foot-shaking on the handover of the Intubation units at Livingstone Hospital are Cecil Frost (Shibah Engineering), Dr Marnè Page, Dr Lorenzo Boretti & Dr Lynn-Hay Frewen
July-August - Expanding the Footprint
Norpharm's involvement was to prove fortuituous as they supported not only licencing, manufacture, distribution (with Browning Surgical) and marketing but they facilitated a Patent Registration (2020/04477) on the unit as well to secure the unit being copied by unscrupulous agents.
To date, 16 units have been delivered to the Livingstone Hospital with many more on the horizon, with the intention of expanding the units footprint across the country as well as globally. The following video gives a nice overview of that process to date.
Contributors (Thanks & Appreciation)
Huge thanks & appreciation must go out to all these individuals for their completely selfless contribution to this, be it for information, advice, their time, their contacts, their services, or whatever contribution they made, no matter how small. Every single one of you answered the call without hesitation and our a credit to our community.
AEDG Team (Clive Hands, Dr William Rall, Zaahid Imran, Jode Fourie, Daniel Trask, Sthuthi Varghese, Blessed Tembo, Charl Rossouw, Zain Imran)
Livingstone Hospital (Dr Bryan Theunissen, Dr Lorenzo Boretti, Dr Marné Page)
eNtSA (Prof Danie Hattingh, Riaan Opperman, Riaan Brown)
Custom Works (Arno Seyfert)
EBET Faculty (Prof Ben van Wyk, Gideon Gouws, Prof Farouk Smith, Dr Anne Lourens, Prof Hannalie Lombard, Mervin Knoesen, Amish Lalla)
Shibah Engineering (Cecil Frost)
NMU Medical School (Philipp Hoelzer, Dr Elizabeth du Toit)
Innoventon (Dr Shawn Gouws)
Black Sheep Industries (Wesley Augustyn)
Nako Triocon (Gideon van den Berg)
Stopforth Robotics Laboratory (Prof Riaan Stopforth)
SAPS (W/O Corne Strydom)